Written by: Dr. Amy Beckley, PhD, Founder and Inventor of the Proov test — the first and only FDA-cleared test to confirm successful ovulation at home.

Medically reviewed by: Dr. Gary Levy, a Board-Certified Reproductive Endocrinologist and OBGYN. Dr. Levy has been the IVF director of a busy, academic, fertility practice. He specializes in complex endocrine and reproductive cases. He is a prolific researcher and author publishing dozens of articles in many prestigious peer-reviewed journals. He also serves as Chief Medical Officer at Fertility Cloud, a comprehensive virtual fertility care platform that helps couples with fertility testing and treatment, all from the comfort of their own homes.
The typical recommendation is that women under the age of 35 try to conceive for 12 months prior to seeking medical care — but why? This is because most fertile couples will conceive within a year of having unprotected intercourse. However, if you have irregular periods, PCOS, recurrent miscarriage, or generally know something is just not right, it can be frustrating and downright destructive to be forced to wait before getting help.
If your body is struggling with underlying problems that may prevent conception, waiting 12 months is not going to solve that. In fact, waiting might physically make infertility challenges worse due to the stress and disappointment from seeing month-after-month of BFNs.
I had this very experience myself. I suffered for more than a year, which included 4 pregnancy losses, before I was “allowed” to seek treatment. By the time I finally got into the doctor, I was so desperate to hold my baby in my arms that when I was presented the option of continuing to try to figure out what was wrong in exchange for a 5-10% chance of successfully conceiving each month versus going straight for in-vitro-fertilization (IVF) with a 70% chance of success, I immediately jumped at IVF.
What I learned a few years later after two rounds of IVF (one unsuccessful, the other resulting in my son) was that my infertility was caused by an ovulatory disorder (i.e. low progesterone). With a $200 supplement, I was able to conceive and carry my daughter to term without issue.
It was this experience that led me to be so incredibly passionate about ovulation health and to invent the Proov PdG test, which is the first and only FDA cleared, rapid response PdG test that allows women to confirm successful ovulation at home. My road to treatment was long, hard, and depressing and I want to save as many other women as possible from having the same experience I did.
Why is progesterone so important?
Doctors don't usually say the word “progesterone” often, but progesterone is the hormone released after ovulation and is needed to support a pregnancy. The most common cause of infertility is no ovulation or ovulation followed by an inadequate production of progesterone (something that here at Proov we refer to as “weak” ovulation).
This means you are not producing progesterone or enough progesterone to ensure the best chances of conception. The good news is that there are many easy ways your doctor can tell you how to increase progesterone if you are not making enough.

There are many easy ways your doctor can help you produce adequate amounts of progesterone if you are not making enough.
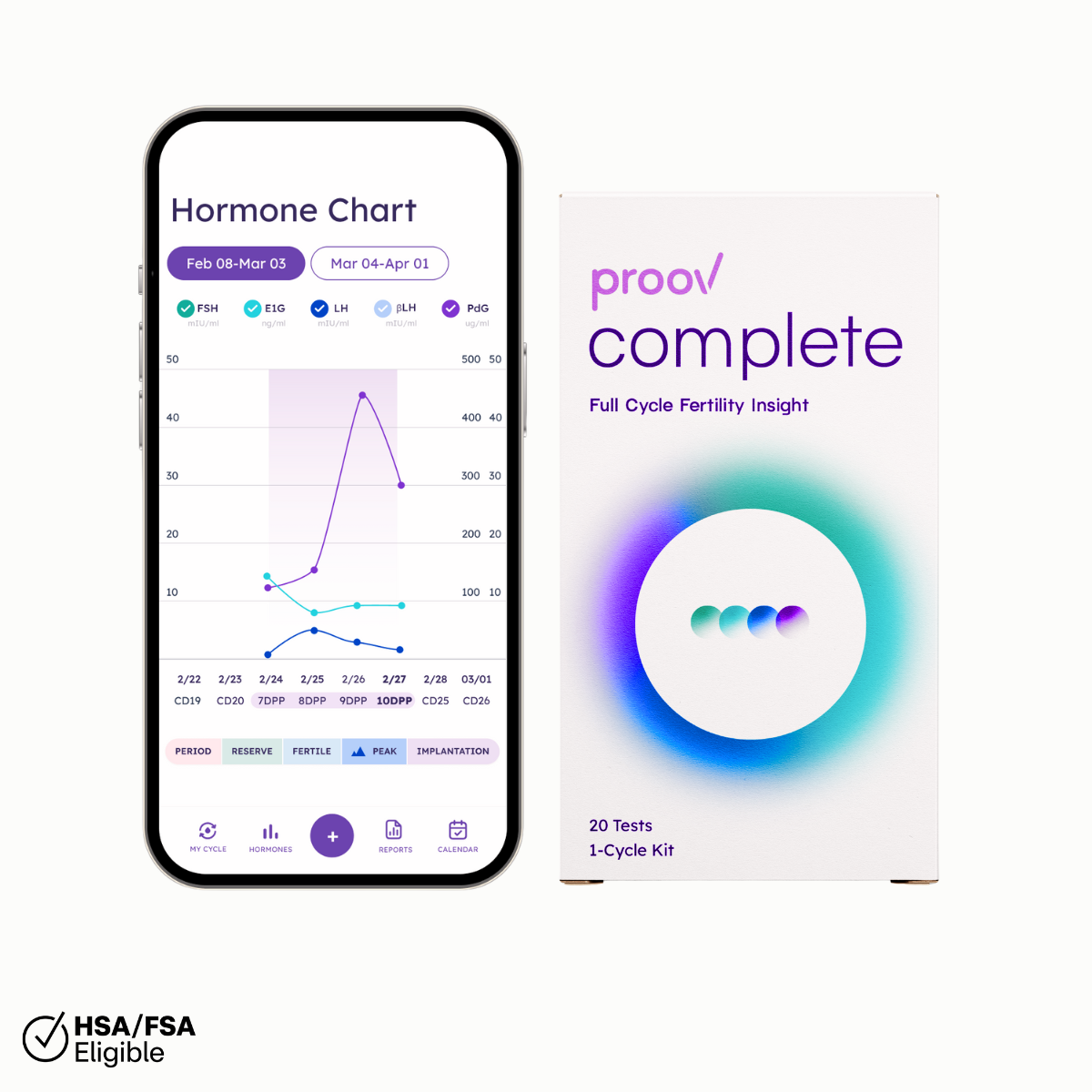
How can Proov help me learn about my PdG?
Proov PdG tests are over-the-counter and can be taken the very first month you are trying to conceive. No waiting an arbitrary 12 months, no doctor's appointment — just you, your bathroom, your urine, and five minutes a day.
Proov PdG tests are designed to show a positive result when PdG levels are at the widely accepted minimum threshold for supporting conception (5 ug/ml, which correlates to about 10 ng/ml of progesterone in blood).
In the first half of the cycle, progesterone is not actively secreted and levels are low. This means PdG is also low and your Proov PdG test will be negative; in other words, you will see 2 lines on the test.
As progesterone and PdG both rise after ovulation, the second line (the test line) will get lighter and lighter until it completely disappears. When trying to conceive, it’s important to ensure PdG is elevated for a few days during the luteal phase, which is typically on days 7-10 after peak fertility. Proov protocol recommends testing daily during this critical 7-10 day window to ensure you are producing enough PdG for long enough to allow for the best possible chance at conception.
If your test is positive, then amazing! You can feel confident that your ovulation is healthy and your body is producing adequate amounts of PdG in order to successfully conceive.
If your test is negative, that’s OK too. You now have identified a possible cause of your infertility. You are armed with valuable information you can take to your doctor and ask them better questions and get better treatment.
What should I do if I have low progesterone?
Low progesterone production (or formally termed, luteal phase deficiency) is treatable. There are multiple ways your doctor can treat ovulatory disorders or insufficient ovulation (luteal phase deficiency).
The following are common treatments for low progesterone you can discuss with your doctor.
1. Ovulation inducing medication
Ovulation inducing medication is usually the first medications doctors try if they suspect you have an ovulatory disorder. These medications help you to ovulate if you are not ovulating and/or produce “stronger” ovulation if you are ovulating, by acting to increase your progesterone levels.
These types of medications work by tricking the body into thinking there is not enough estrogen. This feeds back to the ovary and causes it to start maturing follicles (eggs) in order to increase estrogen levels.
Due to the higher hormone levels, the stimulated follicles are more likely to release a mature egg and more likely to produce a higher quantity of progesterone after ovulation.
2. Trigger shots or hCG Injections
This is slang for a medication that “triggers” ovulation and is usually in the form of purified human chorionic gonadotropin (hCG) that is injected subcutaneously to stimulate ovulation. HCG functions in lieu of your natural LH surge to complete the maturation of a follicle and subsequent release of the egg (ovulation).
The hCG also stimulates the corpus luteum (the empty follicle after it releases the egg) to continue to produce progesterone. Therefore, trigger shots can be used to induce ovulation and potentially stimulate more progesterone production.
Trigger shots can also be used after ovulation to continue to stimulate the corpus luteum to produce progesterone. Some treatment protocols call for two hCG shots to be administered: one to induce ovulation and start progesterone production, and a second one 7 days later to boost progesterone production.
3. Progesterone supplements
Bio-identical progesterone is widely available and a good way to give your body more of the good stuff if you aren't making enough.
In some cases, over-the-counter progesterone creams may be effective. However, if you have a sufficient progesterone deficiency, creams likely won’t be strong enough. (If you choose to opt for creams, we also recommend considering progesterone oils, which can be better absorbed by the skin.)
For women with weaker ovulation (2 or more negative Proov PdG tests), we recommend a prescription level supplement provided by your doctor. Progesterone supplements for fertility are most effective at preparing the body for conception if taken right after ovulation.

Progesterone supplements are most effective at preparing the body for conception if taken right after ovulation.
4. IVF
IVF procedures produce a state of artificial luteal phase deficiency and most, if not all, involve supplemental progesterone. Most of the time progesterone is given via intramuscular injection with a large needle right to the booty. But why?
Well, when the eggs are retrieved after stimulation, doctor’s use an aspiration needle to suck them up. When they do, sometimes parts of the corpus luteum, the progesterone producing cells, also come along too. And since progesterone is so critical for conception, doctor’s always supplement the women’s natural progesterone production with additional progesterone to maintain high pregnancy rates.
5. Dexamethasone
A few clinics use dexamethasone (a glucocorticoid) as part of their treatment protocols. It is also often part of IVF treatment plans.
Dexamethasone is a synthetic form of cortisol. It has several functions, the most common of which is to reduce inflammation. Although not completely understood, dexamethasone can play a role in preparing the uterus for conception by reducing inflammation and increasing the receptivity of the uterus to the embryo.
Since the job of progesterone is to prepare the uterus for embryo implantation, it is thought that dexamethasone likely makes the ovary more sensitive to ovulation inducing drugs or helps progesterone to function more effectively.
Why wait if you don’t have to?
I invented Proov to give women more information about their ovulatory health. When I started trying to conceive, I had so many questions and very little answers — and this only got worse as time went on, and I became more and more frustrated and depressed.
I believe women deserve to have answers and options. Using Proov can help provide more information about what’s going on with your body sooner, so you can have more empowered conversations with your doctor.
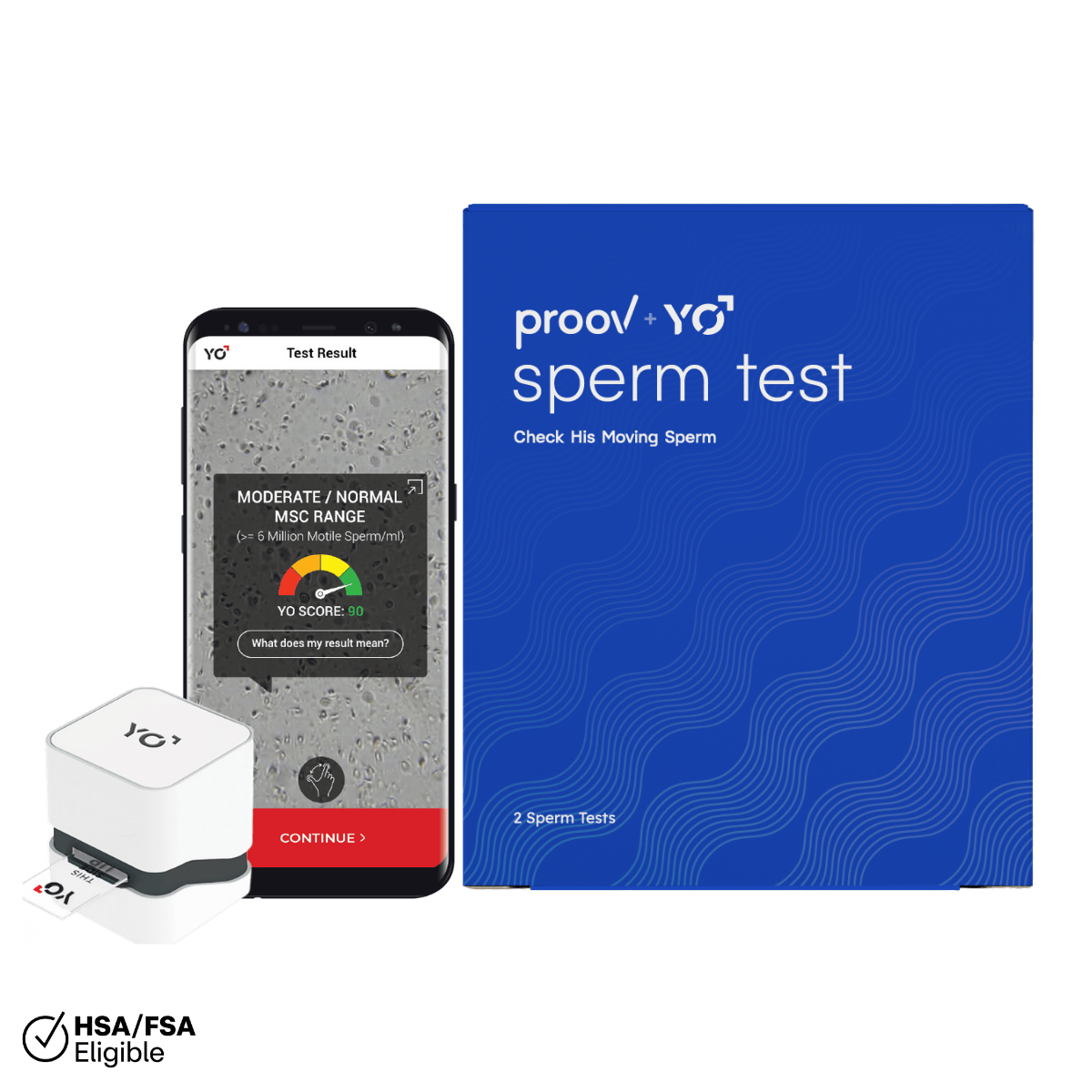
Ready to start your journey with Proov? Order your PdG test kit today!