Written on 4/4/20
Updated on 8/4/22
At Proov, helping women understand the role of progesterone in fertility is more than our company responsibility — it’s a personal mission. That’s because Proov’s founder (that’s me!), directly experienced the huge impact of progesterone on her fertility journey, and started a company to help others do the same.
Through my own experiences, I realized that there’s a lot of misinformation out there about progesterone and fertility, and much of it can be traced back to two specific misconceptions. While you certainly don’t have to be a scientist to benefit from Proov products, getting a handle on the facts about progesterone can be incredibly helpful and empowering when you’re trying to conceive.
In this article, we’ll cover:
- The basics of how progesterone works in the cycle and in early pregnancy
- A common myth about progesterone and ovulation
- A common myth about progesterone testing and measurement
- How you can put progesterone knowledge into action on your own fertility journey
Why is progesterone important?
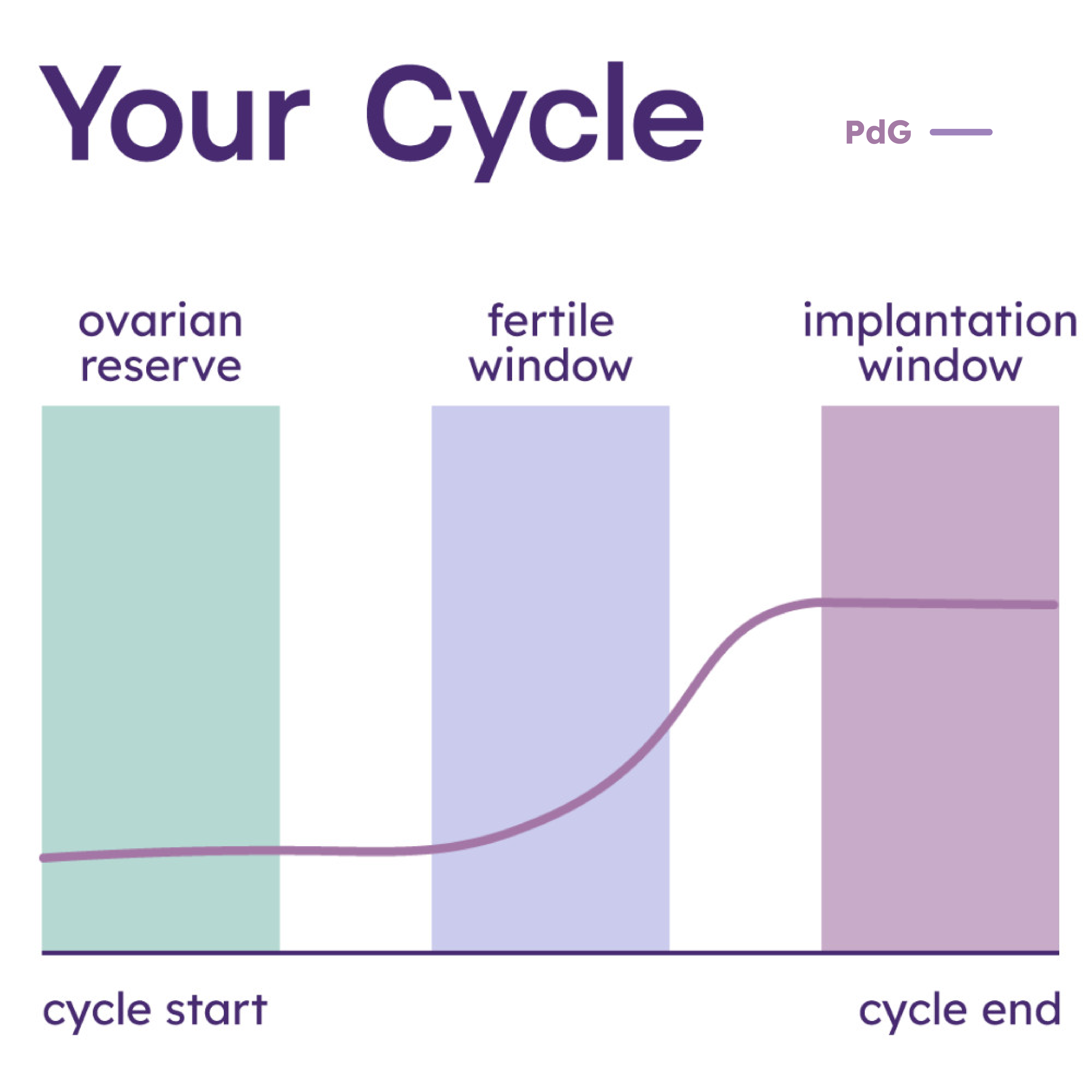
It’s pretty common knowledge that for conception to occur, the ovary must first release an egg from a mature follicle — that’s ovulation. Progesterone is the hormone produced by the empty follicle (also called the “corpus luteum”) after ovulation occurs.
Its job is to make the uterus “sticky” enough to allow a fertilized egg to implant. Progesterone levels after ovulation also creates a healthy uterine environment in which a growing embryo can thrive.
In other words, when it comes to fertility, the release of the egg is just the beginning of the story. A successful ovulation requires adequate progesterone levels, too. At Proov, we define “successful ovulation” as an ovulatory event in which an egg is released and progesterone levels remain adequately elevated throughout the implantation window to provide optimal conditions to support a healthy pregnancy.
When ovulation occurs but is not successful, that can suggest a problem with ovulation that shows up as luteal phase defect or progesterone deficiency. Of course every case is unique, but these conditions are sometimes easily treatable with progesterone supplementation.
Unfortunately this is an area where incorrect information too often stands in the way of the support would-be parents need. Which brings us to Misconception #1.
Misconception #1: Progesterone supplements don't help fix problems with ovulation.
When I suspected I had a luteal phase defect and asked my doctor for a progesterone supplement, he gave it to me — not because he thought it would work, but because taking the supplement wouldn’t harm me. Within two cycles, I was pregnant with my daughter.
My doctor’s lack of faith in the effectiveness of progesterone supplements stemmed from a specific 2015 study that followed 836 women who were trying to conceive. Of the women who observed a positive pregnancy test, half were given vaginal progesterone supplements, and the other half were given nothing. Live birth rates were only 2% higher in the progesterone supplement group, so the study concluded that progesterone supplementation didn’t really help.
But this experiment was flawed. Basic biology tells us that progesterone is required to prepare the uterine lining for implantation, which is why it kicks in right after ovulation, well before implantation actually occurs.
By the time a positive pregnancy test is observed, the embryo has likely already implanted. But if progesterone levels chart came up low during the critical period before implantation, the uterine environment may have never actually reached optimal conditions to sustain a healthy pregnancy, raising the risk of pregnancy loss. In other words, correcting progesterone deficiency after confirmed pregnancy is almost “too late” to make a difference.
Given these biological facts, it makes sense that progesterone supplementation in early pregnancy — as in the study in question — did not create a dramatic difference in live birth rates. Yet the study was highly publicized as “proof” of progesterone’s ineffectiveness overall, and that misinformation spread widely to medical professionals and women seeking care.
In 2017, another study was published that tells a different story. In this experiment, women were given progesterone at the start of their luteal phase (3 days after ovulation) to help them achieve adequate levels before a positive pregnancy test. The results of this study showed a 17% increase in live birth rates in women with a history of pregnancy loss who received progesterone supplementation.

Since the body ideally begins producing progesterone immediately after releasing an egg, it makes sense that for those with progesterone deficiency, early supplementation is key to replicating the optimal luteal phase hormone balance to support successful ovulation, conception, and healthy pregnancy.
Fortunately, now we have tools to understand luteal phase progesterone levels more easily than ever — which brings us to Misconception #2.
Misconception #2: A blood test is the best and only way to measure progesterone and confirm ovulation.
If you suspect you do not ovulate, or that your ovulation is unsuccessful (meaning not enough progesterone is produced after the egg is released), your doctor may order a cycle day 21 progesterone blood test. A day 21 progesterone blood test (also called a “serum progesterone test”) aims to measure progesterone at the point in your cycle when it should be reaching an optimal level to support implantation, about 7 days after ovulation occurs. However, there are a few reasons a blood test can fall short.
First, a serum progesterone test on cycle day 21 assumes you ovulated on day 14 of your cycle. However, every cycle is different, and typical length can vary from 21-35 days. So your cycle day 21 blood draw may not actually fall 7 days after ovulation, and could give you misleading information about your levels.
Additionally, since some fluctuation in progesterone levels day to day is normal, a single serum progesterone measurement doesn’t always show the full picture. In my case, my blood progesterone levels typically looked high around cycle day 21, so I knew I was ovulating. Yet I eventually learned they were dropping prematurely, so my ovulation was not, in fact, successful. A one-time blood test, even if repeated monthly, cannot reveal this type of pattern.
In addition to fluctuating day-to-day in the luteal phase, blood progesterone levels also fluctuate hour-to-hour. That’s because progesterone is secreted into the blood in pulses. Studies have shown that serum progesterone levels can fluctuate 8 times over a single day, ranging from 3-30ng/ml, depending on what time of day you draw blood.
Using a blood test, your progesterone levels might look great at 8am, but by 4pm that same day they could be low. This makes it extremely difficult for doctors to determine whether your serum progesterone levels are consistently high enough to support successful conception.
Another option: understanding successful ovulation with PdG testing at home.
If you’re trying to conceive, progesterone is a key piece of the fertility puzzle. And the good news is that now there’s a great way to understand progesterone levels on your own with easy self-testing for PdG — a marker or metabolite of progesterone found in urine.
Proov Confirm PdG tests are the first and only FDA-cleared PdG tests to confirm successful ovulation at home. Proov Confirm is a simple, non-invasive urine test that’s easy to use each day during the all-important implantation window. Using Proov tests and the Proov Insight app, you can collect your own data to look for the sustained elevated PdG levels that indicate successful ovulation.
Unlike blood tests that measure progesterone directly, Proov works by measuring PdG, a marker of progesterone detectible in urine. Studies show that PdG levels in first morning urine reflect an average of the serum progesterone levels from the day before. Because PdG reflects an average, it’s actually a better way to measure overall progesterone production than blood testing, which only shows the serum progesterone level for a single moment in time.
Testing PdG at home is a great way to confirm successful ovulation, or identify concerns early so you can get the help you need. At Proov, we know first-hand that knowledge is power. The more you know about your levels, the more control you have in your own fertility journey — and we’re here to help!