What Does it Mean to be Postmenopausal? Postmenopause Symptoms & Treatments
If you’ve recently entered postmenopause or are nearing the end of perimenopause, congratulations—you’ve reached an exciting and liberating phase of life! Postmenopause offers the opportunity to focus on your personal well-being, but it’s natural to have questions about what it means to be postmenopausal and how to navigate the changes ahead.
This guide covers everything you need to know about postmenopause symptoms, health risks, and effective treatment options so you can feel confident and supported during this stage.
What is menopause? What is perimenopause?
Menopause is defined as having gone a year (12 months) without having a period, vaginal bleeding or spotting. It marks the end of menstruation and a woman’s reproductive years. Perimenopause, on the other hand, is the transition period leading up to menopause. It typically affects women in their late 40s to 50s, though it can happen earlier.
During perimenopause, your ovaries release eggs unpredictably and infrequently, causing your hormone levels to fluctuate and resulting in symptoms like irregular periods, hot flashes, mood swings, and sleep problems.
What does it mean to be postmenopausal?
Postmenopause refers to the stage of life after you’ve gone 12 consecutive months without a menstrual period, officially marking the end of menopause and your reproductive years. Once you’re postmenopausal, your ovaries stop releasing eggs, your periods and PMS are gone for good, and your hormone levels stabilize at lower levels.
So, how long does postmenopause last? Unlike perimenopause, which is a temporary transition that lasts a few years, postmenopause lasts for the rest of your life. While most menopause symptoms eventually subside, some postmenopausal symptoms may persist or even begin anew. Understanding and managing these symptoms is key to maintaining your quality of life.
Common symptoms of postmenopause

Every woman’s postmenopause journey is unique, but some common symptoms include:
- Hot Flashes & Night Sweats: These sudden waves of heat can persist beyond menopause, especially at night, disrupting sleep.
- Sleep Problems: Insomnia or difficulty staying asleep is often linked to night sweats.
- Fatigue: Persistent tiredness, even after a full night’s sleep.
- Mood Changes: Increased irritability, anxiety, or even depression can occur.
- Skin Changes: Dryness, itching, acne, or sagging skin caused by reduced estrogen levels.
- Weight Gain: Hormonal shifts may lead to weight gain, particularly around the abdomen.
- Vaginal Dryness: Thinning of the vaginal lining can cause dryness, irritation, or painful sex.
- Decreased Libido: A drop in sexual desire is common and often tied to physical or emotional discomfort.
If these symptoms sound familiar, know you’re not alone—and there are many ways to manage them.
Health risks in postmenopause
Understanding the potential health risks that come with postmenopause can empower you to take proactive steps—like scheduling annual physical exams, getting regular preventative screenings, and adopting healthier lifestyle choices—to protect your health, allowing you to focus on enjoying and navigating other aspects of your life. These risks include:
Osteoporosis
Sometimes called the ‘silent thief’, osteoporosis is a metabolic bone disease that happens when there’s an imbalance between the rate at which old, mature bones are broken down and the rate healthier bone tissues are formed, resulting in a loss of bone mass. It is characterized by bone weakness and an increased risk of fractures (broken bones). Except for subtle early signs like back pain, decreased height, brittle nails, receding gums, and tooth loss, osteoporosis often goes unnoticed until the affected person breaks a bone from a minor fall or even coughing.
Typically, estrogen helps to regulate bone metabolism by reducing the breakdown of mature bone tissues and maintaining the formation of new, healthier ones. After menopause, women are particularly susceptible to osteoporosis due to the drop in estrogen levels. It's a good idea to talk to your doctor about bone density testing to assess your current risk.
Heart disease
Women are said to develop heart diseases later than men due to the cardioprotective role estrogen plays in their reproductive years. After menopause, the risk of heart disease increases, often manifesting as higher blood pressure, elevated levels of low-density lipoprotein (LDL, or "bad" cholesterol), which can build up in the arteries, and lower levels of high-density lipoprotein (HDL, or "good" cholesterol). Reduced estrogen levels also lead to changes in body fat distribution, causing fat to be stored around the waist rather than the hips and thighs. This change can lead to abdominal obesity and further increase risk of heart disease.
Endometrial cancer
Endometrial cancer is a type of cancer that begins in the endometrium — the inner lining of the uterus (womb). It typically affects women after menopause. A recent study revealed that 90% of postmenopausal women with endometrial cancer reported vaginal bleeding before their diagnosis; it is an early warning sign. If you notice any unusual vaginal bleeding or spotting, you should contact your doctor immediately.
How can I treat my postmenopause symptoms?

There are many ways to manage postmenopause symptoms. Here are a few options:
Hormone replacement therapy (HRT)
Hormone replacement therapy (HRT) is commonly used to treat the uncomfortable symptoms of postmenopause and support women's overall health during this stage. It works by replacing the hormones, particularly estrogen and progesterone, that the body no longer produces after menopause. Aside from symptom relief, hormone therapy may help reduce your risk of osteoporosis or breaking a bone, heart disease, endometrial cancer, and other chronic diseases. Though, it also comes with risks. It’s important to discuss with your doctor the potential benefits and risks to determine whether HRT is right for you, which type is best suited to your needs, and to develop a personalized treatment plan based on your medical history and symptoms.
Lifestyle changes
Adopting a healthy lifestyle can go a long way in managing postmenopausal symptoms. Eating a balanced diet, exercising regularly, and practicing stress management techniques like yoga or meditation can help you maintain a healthy weight, support your heart, bone, and joint health, reduce stress, improve your sleep quality, and promote overall well-being. When you feel good from the inside and confident about how you look on the outside, you may experience fewer postmenopausal symptoms and feel empowered to manage those that do occur.
Supplements
Calcium, vitamin D, and omega-3 fatty acids are essential for supporting bone and heart health, especially for postmenopausal women who are at increased risk of osteoporosis and heart disease. Women aged 19 and older are advised to receive 1000–1500 mg of calcium, 400–800 IU of Vitamin D, and 1.1 g of omega-3 fatty acids daily. If you are not already getting enough of these nutrients, it’s not too late! Taking supplements can help fill any nutritional gaps, ensuring you meet the daily recommended amounts.
Vaginal estrogen therapy
For postmenopausal women experiencing vaginal dryness, dyspareunia (pain during sex), and some urogenital symptoms (like urinary urgency), vaginal estrogen administered locally—that is, directly on the affected area—through low-dose estrogen creams, rings, gels, or tablets can provide significant relief. In fact, It has been shown to decrease the number of recurrences per year among postmenopausal women with recurrent UTIs.
Over-the-counter (OTC) vaginal lubricants
These non-hormonal alternatives to vaginal estrogen can help relieve vaginal dryness and discomfort during sex. Though lubricants are a temporary solution, they can be used in combination with other treatments for better and more impactful results.
How do I know I’m in postmenopause?
If you’ve gone a full year (12 months) without a period, you have officially entered menopause and are now considered postmenopausal. If you are unsure about your status, you can ask your doctor for a blood test to check specific hormone levels, which can confirm whether you’ve reached menopause.
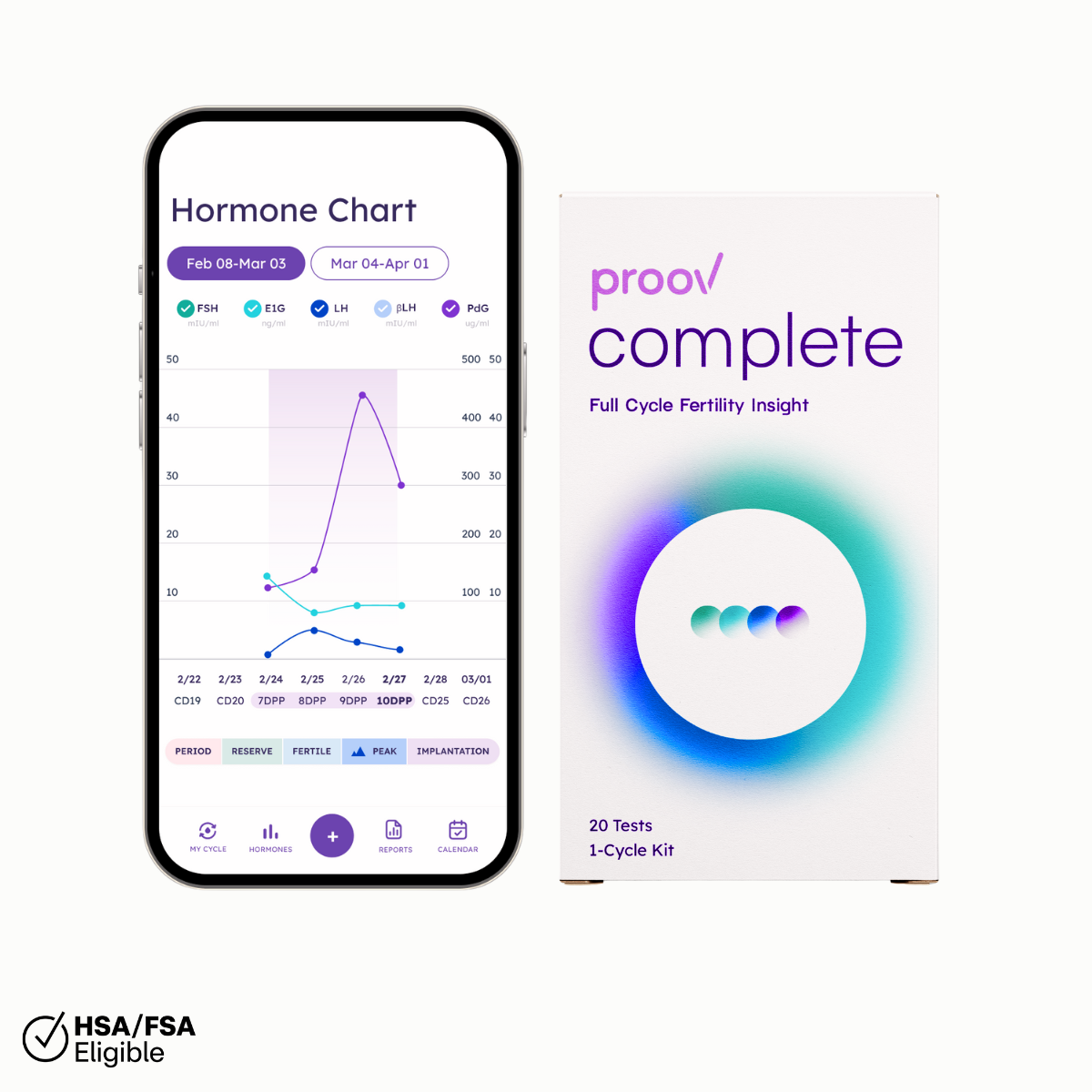
Proov Empower can help you find out what stage you are in and navigate your journey with confidence and ease. With our just-pee at-home hormone tests, which are accurate and non-invasive, and free companion app, you’ll have all the actionable insights needed to manage your symptoms and stay in control—anytime and anywhere. No need for constant doctor visits. No blood work required.
Our comprehensive support system will help you feel truly supported every step of the way. We offer natural solutions—like the Boost Herbal Supplement, which supports estrogen production—to support your journey, as well as quality customer care from a team of women who are available seven days a week to provide timely support. You will also have access to an online community of women who share similar experiences. If you need tailored expert advice or prescription medication support, we can also quickly connect you with a medical expert.