Proov founder and PhD Scientist, Amy Beckley, recently listened to a presentation from a reproductive endocrinologist. He spoke about his practice and fertility. When he asks a patient, “Is your cycle regular?” and she answers, “Yes,” he automatically assumes she is ovulating properly and begins to look for other causes of infertility.
Amy believes this is a mistake. But why?
In this case, “regular” means your cycle lasts for a consistent number of days, cycle to cycle. Knowing this is like tracking the bare minimum - it tells you nothing about your hormones, ovulation, or if your body is prepared for conception.

Different Types of “Regular” Cycles
A recent study published a chart which depicts estrogen and progesterone levels during seemingly “regular” cycles. We’ve chosen a few important cycle patterns so that we can see how little a “regular” cycle tells us about the health of ovulation or hormone levels.
Regular Cycles without Ovulation (aka Anovulatory Cycles)
Anovulatory cycles with fluctuating estrogen levels: In the above cycle, there is an estrogen surge but no lh surge. Estrogen levels (green line) will start to rise, but they never get high enough to induce a luteinizing hormone (LH) surge and trigger ovulation. However, we see somewhat “regular” drops in estrogen, which occur after failed ovulation attempts. Anovulatory cycle hormone levels and drops can cause menstrual bleeding, leading a woman to believe her cycle is normal. In reality, estrogen is too high and ovulation never happens, which means that there is no empty follicle to produce progesterone (yellow line). In this cycle pattern - most commonly found in women who are breastfeeding - conception is not possible.
Cycles with anovulatory ovarian activity with constantly increased estrogen levels: In this cycle, estrogen and LH levels are both high, but they never trigger ovulation. As we previously saw, high estrogen levels with no ovulation or progesterone production means that conception can’t happen. This pattern is most commonly found in women with Polycystic Ovarian Syndrome (PCOS). In many women with PCOS, cycles will be “irregular” meaning that they are longer than usual. However, some women still experience a menstrual bleed about every 30-35 days which can lead to them being lumped into the “regular” bucket.
Cycles with a luteinized unruptured follicle: This is another cycle pattern where we see elevated estrogen and LH. This time, these elevated levels trigger a follicle to prepare for ovulation, but an egg is never actually released. We can see the follicle produces a little bit of progesterone in preparation for ovulation, but since an egg is never released, progesterone never reaches an optimal level. This type of condition is called a Luteinized Unruptured Follicle (LUF). This type of cycle activity is most commonly found during the perimenopausal period, hyperprolactinemia, and infertility. In this cycle pattern - as you probably guessed - conception is not possible.
Regular Cycles with Suboptimal Ovulation
Cycles with ovulation followed by a deficient luteal phase: In this type of cycle, estrogen and LH are elevated, triggering ovulation. However, progesterone levels after ovulation are low and/or drop too soon. In this pattern, ovulation occurred and an egg was released, but low progesterone makes conception difficult, as progesterone prepares the uterine lining for implantation. Without this preparation, a fertilized embryo cannot survive. This type of pattern can be found after breastfeeding during the period of returning fertility, in women with infertility, during the menopausal transition, and in women with hypothyroidism or hyperprolactinemia.
Regular Cycles with Successful Ovulation
Ovulatory cycles with adequate luteal phases: We’ve reached the good stuff! During this type of cycle, there is an adequate hormonal balance between estrogen and progesterone. An egg is released and hormone levels are best suited to support conception.
Know More About Your “Regular” Cycle

When the hormonal balance between estrogen and progesterone is disrupted, ovulation may not occur and women are at a greater risk of experiencing infertility, even if their cycle seems “regular.” Therefore, monitoring ovulation gives you more valuable information about your cycle and body!
In all the cases above, progesterone levels were the best indicator of successful ovulation, since we saw that an estrogen surge before ovulation didn’t always mean an egg was released. Progesterone can be measured via a one-time, cycle day 21 blood test at your doctor’s office. But since progesterone levels need to stay elevated post-ovulation, ensuring adequate levels across your cycle requires multiple blood draws.
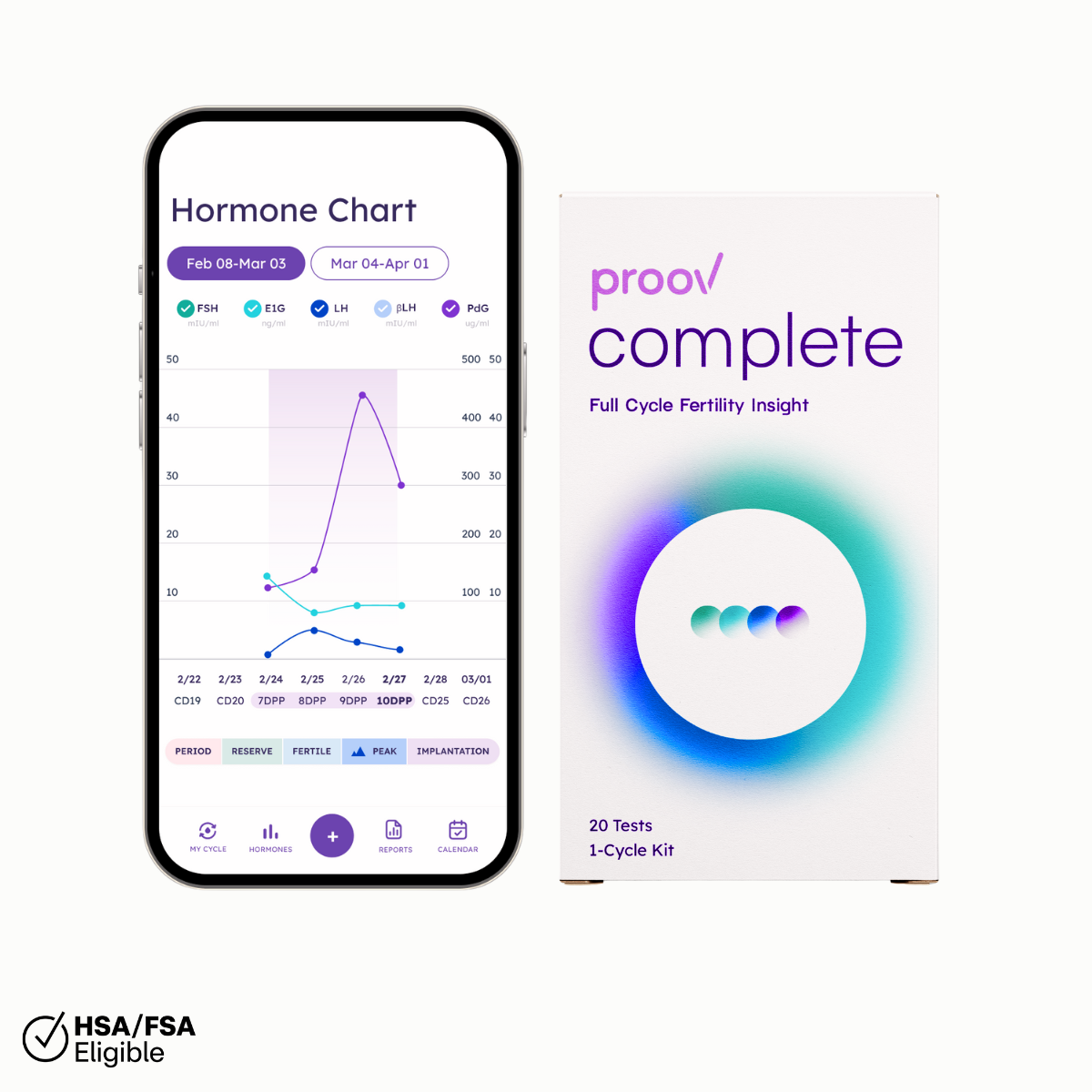
But don’t worry! Proov makes confirming ovulation at home easier, helping you avoid those pesky needles and multiple trips to the clinic. Proov measures PdG – metabolite of progesterone – in first morning urine and a positive Proov test confirms ovulation. Additionally, positive Proov tests days 7-10 after suspected ovulation confirm successful ovulation, like we saw in the final cycle pattern. Confirming ovulation with Proov helps take some of the mystery out of your “regular” cycle!