Written by: Dr. Alison Gottschalk ND
Written on 9/23/21

Dr. Alison Gottschalk talks about what you need to know about polycystic ovarian syndrome when trying to conceive.
Have you been diagnosed with polycystic ovarian syndrome (PCOS)? You may have heard that women with PCOS have a harder time conceiving.
While this can be true, there are many steps you can take to manage your PCOS. Here’s what you need to know about polycystic ovarian syndrome when trying to conceive.
What is PCOS?
Polycystic ovarian syndrome is a women’s health concern that — despite the name — does not require you to have cysts on your ovaries. Simply put, PCOS is considered both a complex metabolic concern, as well as a complex hormone concern.
This is because in most cases, we see a disturbance in blood sugar regulation (a metabolic issue) along with hormonal imbalances. Often, the hormonal imbalance involves elevated levels of testosterone and lower than normal levels of estrogen and progesterone. This is often caused by a lack of ovulation.
As a condition thought to impact 1 in 10 women globally, it’s quite shocking how under-the-radar this concern has gone. You can test this out for yourself by asking a girlfriend if she’s ever heard of PCOS — you may be surprised with how little information is out there.
How do I know if I have PCOS?
It’s important to understand the main symptoms of PCOS so you can identify them and bring any concerns to your doctor. The main symptoms that lead to the discovery of PCOS are usually:
- Difficulties trying to conceive or a history of recurrent miscarriages
- Long cycles, usually exceeding 35 days or having less than 10 periods per year
- Difficulties trying to lose weight
- Cystic acne, especially if it’s resistant to medications like Accutane (Isotretinoin)
- Hair growth on face, jawline, chin, or below the belly button, also called hirsutism
- Hair loss on the top of the head, also called androgenetic alopecia
If you think you may have PCOS based on the symptoms above, it’s best to look at the most widely accepted diagnostic criteria for PCOS called the Rotterdam Criteria. This criteria requires you to have 2 out of 3 of the following:
- Elevated testosterone on your blood report (what we call a biological marker) or elevated testosterone symptoms (which is a clinical marker)
- Cycles that are 35+ days in length, or having less than 10 periods per year
- Cysts on your ovaries, discovered via ultrasound
If you are concerned about PCOS, I recommend consulting your healthcare provider and asking for tests per the above criteria.

If you think you may have PCOS, it’s best to look at the most widely accepted diagnostic criteria for PCOS called the Rotterdam Criteria.
How is PCOS treated?
As a women’s hormone & PCOS Fertility naturopathic doctor, many of my patients come in to see me reciting a similar story. They usually have irregular cycles, troubles trying to conceive, or difficulties with weight loss.
Often, they turn to Google to better understand their new diagnosis. In most cases, these patients are either offered the birth control pill or are told to “exercise more” and “eat less sugar” to better manage their PCOS.
The reality is there is so much more we can offer women than just the birth control pill. Keep in mind that the birth control pill does not balance your hormones; rather it suppresses your natural hormone production.
There can be benefits to being on the pill with PCOS, as the pill can decrease elevated testosterone levels, lessen the severity of cystic acne, irregular cycles, and facial hair growth in the short term. However, it’s usually not until the pill has been discontinued when we see the full extent of the hormone imbalance that has been masked by the pill.
It’s usually when the pill has been discontinued and women are ready to start trying to conceive, when troubles with conception arise, as we see this reemergence of the hormone imbalance that initially brought them to the pill.

The reality is there is so much more we can offer women rather than just the birth control pill.
Can you get pregnant with PCOS?
It is absolutely possible to get pregnant with PCOS. One of the main reasons it may be more difficult, however, is because of a lack of ovulation and the hormone imbalances caused by this lack of ovulation.
My approach to PCOS fertility is to first determine what is preventing you from ovulating with PCOS. The most common reasons why we see a stall in the ovulatory process is due to elevated testosterone, inflammation, cortisol, or low thyroid hormone levels — all of which are essential for conception and maintenance of pregnancy in that first trimester.
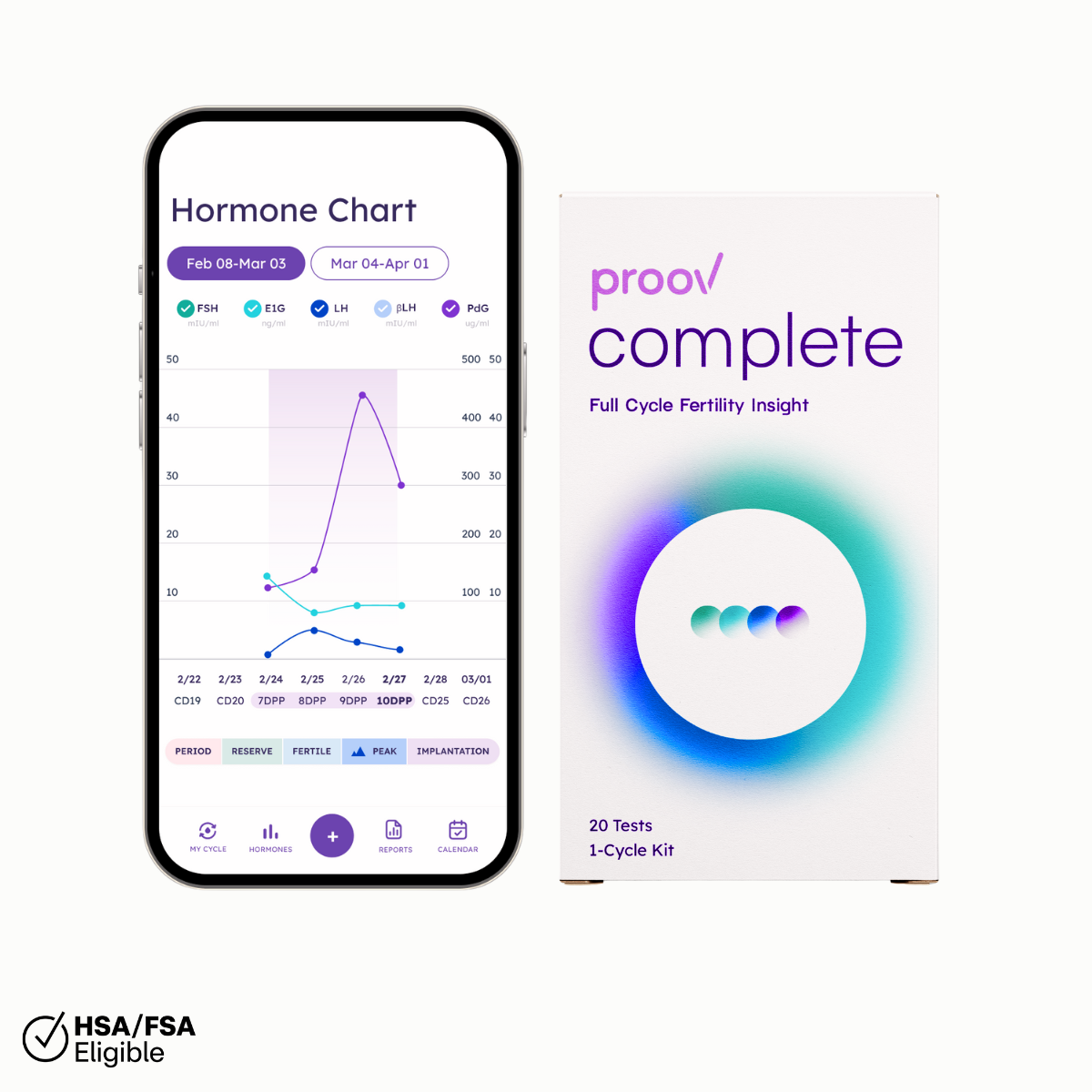
Determining your PCOS ovulatory blocks, will determine the direction of our treatment approach. As a first step, we first need to confirm that you are in fact ovulating successfully. This means eggs are being released each cycle and PdG (progesterone marker) levels are remaining adequately elevated for long enough to allow for the best possible chance at conception.
To do this, we can use Proov Confirm, the first and only FDA cleared PdG test to confirm successful ovulation at home. Testing with Proov Confirm 7-10 days past peak fertility is a great way to have a better understanding of your ovulation, and provides great information for a doctor like myself.
There is so much more we can offer women with PCOS than just the pill or “exercise more” and “eat less sugar.” For more PCOS fertility support, please download my free PCOS Fertility guide.
Want to learn about my favorite supplements for PCOS? Head over to the private Proov user and support Facebook group to watch my live video with Proov founder, Amy.