Written by: Hannah Bowers, an Integrative Nutrition Health Coach, Certified Lactation Counselor, and writer who is passionate about providing evidence-based resources for preconception, pregnancy, and postpartum.

If you’re currently breastfeeding – or considering breastfeeding – you may be wondering how this feeding choice will impact your fertility. Lactation Amenorrhea Method (LAM), or the lack of a menstrual cycle due to breastfeeding, is a well known concept, but many confusing ideas persist about how (and if) it impacts fertility.
In this article, we’re going to explore how breastfeeding can impact fertility and what you must know when trying to conceive again. Read on for all the details!
So, how does breastfeeding impact fertility?
Prolactin is a hormone secreted by the Pituitary gland to stimulate milk production. This is easy to remember because prolactin and produce start with the same three letters.
High levels of this hormone suppress reproductive hormones, temporarily pausing ovulation and menstruation. Frequent suckling, specifically, is what triggers the pituitary gland to increase levels of prolactin and make more milk.
What’s interesting to note here is that elevated prolactin, even outside of breastfeeding, can cause cycle dysregulation. Hyperprolactinemia, or the presence of unusually high prolactin, is routinely screened for in women with infertility.
This condition can be caused by a variety of factors, ranging from a pituitary tumor to thyroid disease, but ultimately highlights the impact this hormone has on ovulation.

High levels of prolactin suppress reproductive hormones, temporarily pausing ovulation and menstruation.
Why it’s hard to predict when your cycle will come back
When and if your cycle will return while breastfeeding is hard to predict. LAM is generally viewed as effective birth control when the baby is less than six months old and exclusively breastfeeding, and you have not experienced bleeding beyond the initial postpartum period.
Researchers found that exclusively breastfeeding mothers who are nursing frequently often experience a return of fertility between 9 and 18 months postpartum.
Why do some breastfeeding women have shorter or longer periods of LAM? Many habits that are compatible with LAM can impact overall prolactin levels.
Timed or reduced feedings, sleep training/eliminating night feedings, supplementing with formula, and even pacifiers and bottle use, when replacing a breastfeeding session, are all commonly noted to negatively impact prolactin. For example, many mothers experience a return of fertility upon returning to work, due to the sudden change in the breastfeeding frequency.
What can I do to enjoy a longer duration of Lactation Amenorrhea?
If you’re hoping to delay the return of menstruation, there are a variety of things you can do to encourage long term protection through LAM.
Start thinking about breastfeeding during pregnancy.
Mammary glands develop during pregnancy, which is no surprise given the breast changes that occur beginning in the first trimester. Having adequate nutrition encourages the ducts to develop and prepare for the incredible task of breastfeeding. Vitamin A, for example, is noted to be especially important and should be amply supplied through your prenatal and food choices.
Outside of the US, mothers are encouraged to begin expressing colostrum after 36 weeks. This can help to prepare the body for feeding and also provides a supply of colostrum, should early supplementation be necessary. Speak to your care provider to ensure that this is a good fit for your unique situation.
Implement the principles of Ecological Breastfeeding
This approach to breastfeeding models ancestral feeding patterns; essentially, keep the baby close, feed frequently, and avoid the use of artificial nipples (pacifiers and bottles). Sheila Kippley’s book is considered the most reliable text on this topic and outlines each “rule” of preventing the return of fertility in depth.
Be cautious with the rate of postpartum weight loss
While every mother understands the desire to get back in shape, the early postpartum is generally not the ideal time to begin dieting or exercising intensely. Researchers have found that mothers who lose a large percentage of fat early on in the postpartum period are more likely to experience a shorter duration of LAM. This doesn’t mean that you can’t lose weight or get back to being active, simply be mindful not to overdo it.
How can I encourage my body to start cycling again?
If you are past six months of breastfeeding and have yet to experience a return of fertility, you may wonder how to get things going again. Here are a few lifestyle and breastfeeding tweaks that may help to lower prolactin and restart ovulation:
As always, please speak to your care provider before trying to conceive again or making any dietary, lifestyle, or supplement changes.
- Discontinue Any Non-Essential Pumping: Frequent milk removal encourages the prolactin level to remain high.
- Go Back to Work (or Out Solo Regularly): Pumping away from your nursling can result in lower prolactin.
- Eliminate Night Feedings: Night feedings result in higher prolactin levels. It is generally not recommended to eliminate night feedings prior to six months of age, though some experts advocate for holding off until twelve months. Please speak to your child’s care provider and a lactation counselor before night weaning.
- Increase Caloric Intake: Harvard Researcher Rose Frisch found that even a minor weight gain or increase in calories can trigger the onset of postpartum menstruation.
- Consider a Supplement Containing Vitex: Vitex is noted to reduce prolactin levels. Vitex can be found in Proov’s Luteal Love herbal supplement.
Many women will notice a return of fertility after incorporating a few of these changes into their regular routine. That said, women with a history of low body weight or hypothalamic amenorrhea may not experience a return of fertility until after fully weaning.*
The Return of Ovulation & Beyond
The first postpartum cycles could be quite different from what you remember. While some women experience ovulation prior to their first bleed, this is more common in mothers who do not breastfeed. A few breastfeeding mothers will experience an anovulatory cycle while others will have short luteal phases for the first few cycles, primarily due to insufficient hormone levels.
Early changes in cervical mucus can also be misleading, which makes predicting fertility a challenge. While cervical mucus is a useful metric once cycles are occurring normally, researchers have found that it correlates poorly with ovulation until hormones have reached normal cycle levels.
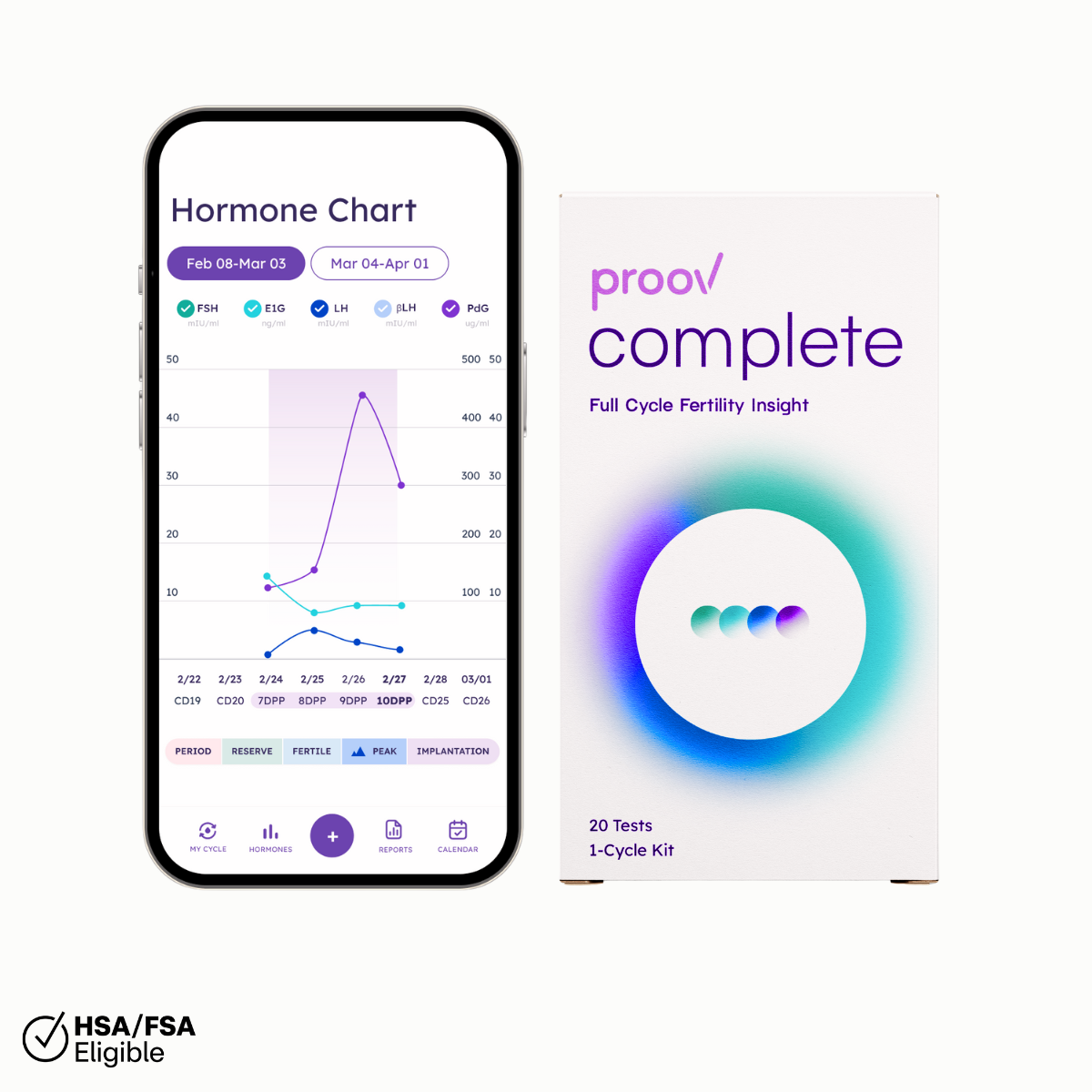
Fortunately, Proov Complete is a reliable option for accurately assessing fertility. This at-home test kit allows you to measure four key fertility hormones from the convenience of your bathroom. Real values are displayed on a chart within the Proov Insight App, allowing you to easily understand what is going on with your hormones.
Once cycles do resume, Proov Complete continues to be a useful test for evaluating the overall cycle. E1G (urine marker of estrogen) and LH (luteinizing hormone) help to predict ovulation while PdG (urine marker of progesterone) confirms ovulation did, in fact, occur. Proov Complete also offers a detailed picture of overall hormone function, fast tracking treatment, should it be needed to get pregnant again.
If you have further questions about your cycle while breastfeeding, we recommend consulting your doctor.
*Mothers who wean and do not see the return of a cycle within a few months should reach out to their care provider for further evaluation.